|
Parents need information, not judgement All parents want to give their babies the best start in life, and nutrition is no exception. Breast milk or formula should be the sole source of nutrition for infants under six months, and should remain the primary source of nutrients until at least 12 months (AAP). While most mothers (83%) in the US start out breastfeeding their babies, less than half are exclusively breastfeeding at three months, and only 25% are breastfeeding exclusively at six months (CDC). This tells us that most families are looking for alternatives to supplement or replace breastmilk within the first six months. There is no shame in this – modern motherhood is HARD! We have virtually non-existent maternity leave in the United States (the only developed nation that doesn’t offer federally mandated paid parental leave), making it more logistically challenging to breastfeed our infants. With around a third of babies being born via C-section, many women don’t have the opportunity to nurse their babies during the first hour after birth, which plays a role in breastfeeding success. And, with complicated deliveries, mother or baby (or both) are busy being treated for complications, or sleeping off meds, so things don’t always get off to the best start. Structural and societal support are also lacking, with only 25% of babies born in hospitals that provide an optimal level of support for lactation (the Baby Friendly designation from WHO and UNICEF guidelines); while this is a significant improvement from a decade ago (only 3% in 2007; BabyFriendlyUSA), it's still not optimal. Plus, in the US we also face a taboo around breastfeeding in public which adds an additional barrier to success. Some women experience low milk supply, or a baby who struggles to latch, or a colicky baby who never seems satisfied. These are things that a lactation consultant can help with, and smooth the (often bumpy) breastfeeding journey, but not everyone has access to one at the right time, place, or price point. Some women are plagued with self-doubt and/or exhaustion at 3 am, or a well-meaning loved one tells them to sleep through the night while they feed the baby, and that little bottle of formula that the hospital sent you home with (“just in case”) is readily available. Some women commit to breastfeeding exclusively for the first six months, then choose to switch to formula for the rest of the first year, and other women decide from the get-go that they won't be nursing, as is their prerogative. Women KNOW that breastfeeding is optimal, and they may have a whole bunch of feelings around the fact that they’re not doing it as much or as long as they'd like - they simply want to know what the best substitute is if they decide that need one. Whatever their reason, most women do not come to the decision to stop nursing lightly and deserve our support in choosing the next best thing for their child. What are the options?
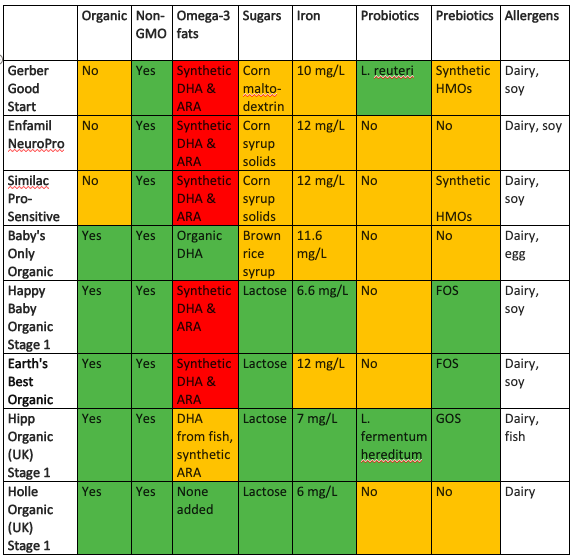
Commercial formulae, deep dive: Plant-based formulae are non-dairy alternatives for babies who struggle with cows’ milk-based formulae and/or families who choose a vegan lifestyle. Soy formula has fallen out of favor recently: most soy in the USA is genetically modified (94%, 1), which is a concern for many parents due to pesticide exposure. There have also been concerns that exposure to high levels of phytoestrogens naturally occurring in soy could be harmful to babies, particularly girls in later life (2). In response to these concerns, the National Toxicology Program's Center for the Evaluation of Risks to Human Reproduction (CERHR) convened an expert panel to evaluate soy infant formula in 2009 and concluded that there was minimal concern for babies drinking soy–based formulae. Regardless, many parents would rather not give their babies controversial ingredients, and a recent newcomer to the market place uses pea protein as an alternative. Organic vs. Conventional: choosing organic means skipping the pesticides, herbicides, and growth hormones that are often present in conventional milk and soy products. That being said, the USA has an increasingly long list of ingredients that are permitted in products certified organic, some of which are from dubious sources. Another designation worth looking out for, in the absence of organic certification, is non-GMO project verified. While GMOs are banned in Europe, in the USA they are generally regarded as safe. GMOs are exposed to higher than normal levels of pesticides and herbicides, toxins which infants’ immature systems have a harder time clearing. There is some observational evidence of a link between exposure to pesticides in utero and infancy and increased incidence of autistic spectrum disorders (3). With studies showing that eating organic does effectively reduce levels of pesticides in our children’s bodies (4), it is worth the extra cost, if you can afford it. Types of fats, including DHA & ARA: the omega-3 fatty acids in breastmilk are one of its selling points, thought to be responsible for boosting babies’ brain health. DHA is a key building block for your baby's brain and eyes, and formula-fed babies have been shown to have lower levels, so it is only natural that manufacturers want to add this to their products. However, most US manufacturers use DHA from algal oil, which is somewhat controversial due to processing methods, plus the benefits of adding this as an isolated ingredient are not well established. The FDA has now expressed some concerns about adding it to formula since approving it in 2002 (5). Artificial ARA and DHA will show up as m. alpina oil and c. cohnii oil in the ingredients list. Some complain that it is synthetic and uses known neurotoxins in processing, therefore shouldn’t be added to any products labelled organic, but it is on the aforementioned list of ingredients that get a pass. Good quality European brands use fish oil as their source for added fatty acids, while some in the US use DHA from eggs. Aside from the omega-3s, the sources of fats in formulae usually include a mix of plant-based fats such as coconut oil, soy oil, canola oil, sunflower oil, and palm oil. Formula is typically slightly lower in fat than breast milk (and slightly higher in carbs and protein). Types of carbohydrate & sugars: breast milk contains lactose, a natural sugar, and complex carbohydrates called human milk oligosaccharides (HMOs) which work as prebiotics – food for the developing microbiota in the babies’ guts. HMOs play a significant role in establishing immune and gut function and protect against pathogens (6). Some formula companies are now adding synthetic HMOs to their products, and industry-sponsored research suggests that this conveys some health benefits (7). Most commercial formulae in the US use simple sugars such as corn syrup, glucose syrup (often from wheat) and sucrose; these are probably from GMO sources unless certified otherwise (look for non-GMO or certified organic). Sucrose isn’t great for teeth, so once baby has a few, you may want to clean their teeth after feeding them formula containing sucrose. Some of the organic brands opt for brown rice syrup instead of other sugars, but brown rice syrup can have high levels of arsenic – one study found that baby formulae with organic brown rice syrup had 20 times the arsenic levels of those formulae not using it (8). Maltodextrin is another controversial additive: a long chain carbohydrate derived from corn or wheat, it can disrupt the gut microbiota, which isn’t what we want during such a critical period of microbiome development (9). Iron: adequate intake of iron for an infant 0-6 months old is 0.27 mg/day; for a 6-12-month-old this jumps to 11 mg/day. Babies’ needs actually increase gradually as the months go by, due to dwindling iron stores (babies stock up in utero, assuming the mother is well-nourished, and the pregnancy is full term). Infants start eating solid foods around six months, which provide a source of iron in their diet. It is worth noting that iron is one of the nutrients where more is not better, in fact, more can be harmful, so we should always supplement with caution. It used to be possible to buy both low iron and high iron formulae (typically 4 mg/L vs. 11 mg/L), but now low iron formulae are harder to find in the US. Lower iron is usually adequate for younger babies (10). If we are looking to nature for our model, mothers’ milk has very low levels (0.5 mg/L), and full-term healthy babies are born with enough stored iron to last the first 4-6 months (or longer if they didn’t have their umbilical cord clamped immediately at birth). Additionally, it takes the gut around six months to mature, and during this time it does a poor job of regulating iron uptake, meaning that a lot of the supplemental iron sits in the developing GI tract, where it may cause constipation and increase susceptibility to GI infections, as well as interfering with absorption of other minerals. High iron formulae are the norm in the US, with almost all brands having ~12mg/L; for comparison, most European brands stick with <7 mg/L, especially for younger babies. It is worth restating that the RDA for younger infants is 0.27 mg/d, which this far exceeds. One of the reasons for this is that the iron in breastmilk is very well absorbed due to an iron-binding protein called lactoferrin, which nature provides to ensure absorption of the naturally occurring iron in breast milk – around 50% of iron from breast milk is absorbed, vs. 7-12% of supplemental iron in formula. Some formula companies add bovine lactoferrin to their formulae to aid with absorption, but there are mixed results about whether this is beneficial. Probiotics: The live cultures in breastmilk are one of the keys ways in which it is ‘better than’ human milk alternatives. Research has shown that breast milk contains over 700 different types of bacteria, including common probiotic strains such as Lactobacillus and Bifidobacterium, as well as Streptococcus, Staphylococcus and Enterococcus. The breast milk microbiota shifts continuously to meet the ever-changing needs of the infant: over the first few months of a baby’s life the concentration of different strains of microbes in their mother’s milk shifts from month to month, and during each nursing session the baby’s saliva transmits information on its health status to the mother’s immune system, allowing for customized defenses at the next nursing session. Because of this, human milk probiotics are not truly replicable, but adding probiotics to formula certainly makes sense, as formula-fed babies are otherwise missing out on this key element of gut and immune development. Probiotic supplements are emerging as a potential way of alleviating colic (e.g. L. Reuteri), and reducing allergies and atopy in infants (e.g. LGG and L gasseri). It might make sense to supplement your baby with these if they're prone to these conditions, but you don't necessarily need it to be in their formula, you can supplement separately with whatever is best suited to your child's needs. Lactobacillus infantis is an important strain that babies get from their mothers during vaginal birth, associated with reduced intestinal inflammation, but recent findings from a probiotic company studying baby poop found that up to 90% of US infants have no L. infantis in their microbiome (11). This is probably due to the increase in c-section deliveries and the use of antibiotics in early life, across generations - if mom doesn't have these microbes, she can't pass them on to her infant. Formulae of the future will likely have many more added as we learn more about the human milk microbiota. That being said, for now it is probably more useful to supplement with a separate multi-strain probiotic that meets the unique needs of your child (e.g. colicky, or risk of allergies, etc), rather than going with a formula advertising that it has added probiotics but usually only has one or two strains. BPA: a plasticizer used in hard plastic bottles and for lining cans, this chemical can leach into liquid formula preparations, but it doesn’t appear to leach into powdered formulae. When it comes to feeding your baby, stick with glass baby bottles to reduce BPA exposure further – bottle-fed babies (whatever they’re drinking) are exposed to more BPA than babies fed at the breast. If you must use plastic bottles (some daycares ban glass), be mindful not to heat them, and hand-wash them to reduce leaching. Water quality: if you are mixing powdered formulae with water, you’ll want to be sure that the tap water in your area is safe to drink. A recent report from the EWG (12) found that 97% of water samples from across the USA were contaminated with PFAS – industrial chemicals that never breakdown, and have been associated with various health concerns (13). This is far more widespread than previously believed. Also, the CDC cautions against regularly mixing formula with fluoridated water, because excess fluoride can discolor emerging teeth. About 70% of people in the US have fluoridated tap water (14), and most water filters don’t remove the fluoride. Another downside of fluoridated water is that it can cause lead to leach from pipes into the water – some studies have found that children drinking fluoridated water have double the blood lead levels of those drinking non-fluoridated water (15). Reverse osmosis filtered tap water or bottled spring water is the best way to avoid this. So, what to do with all this information? There is no one perfect formula, just like there is no one perfect diet – what is best for your baby depends on your baby’s unique needs and what's important to you as a parent. I’ve compiled a reference chart with some of the leading options - these are not ones that I necessarily endorse, nor is it intended to be an exhaustive list, they are simply a selection of the top selling brands, plus some of the leading organic options (domestic and European), to show the variety available, and how they stack up against the criteria discussed above. If you would like personalized guidance on what's best for YOUR baby, or to find out more about what their microbiome might be missing, please contact me, and we can set up a consultation.
1 Comment
7/26/2021 07:18:07 pm
Thank you for sharing this about horse health care tips I learned a lot from this article. I hope you will post more content about horse health. By the way, Wanna share my experience about using Food Supplements for Horses product from France (Genuine Haarlem Oil). Their products are very effective and good for horse health. You can try it also. Thanks!
Reply
Leave a Reply. |
AuthorHi, I'm Amy. I'm a nutritionist in the DC area, working with clients of all ages, focusing on prenatal and pediatrics. I'm all about straightforward, evidence-based health & wellness advice - because life/parenting in the modern world is complicated enough! Categories
All
November 2022
|
Seed to Sapling Nutrition

 RSS Feed
RSS Feed